Today we are talking about telerehabilitation, one of the fastest-growing fields in digital healthcare, closely connected to telemedicine. Patients who have difficulties moving around or who require continuity of care outside the clinical setting can benefit from remote rehabilitation services thanks to modern digital technologies.
Keep reading.
Table of contents
What does rehabilitation involve?
Rehabilitation is generally a multidisciplinary process aimed at restoring, maintaining, or improving physical, cognitive, psychological, or social functions that have been compromised due to illness, trauma, disability, or degenerative processes.
It can include motor rehabilitation (movement, balance, targeted physical activities), neuropsychological rehabilitation (cognitive functions such as memory, attention, and language), as well as rehabilitation of communication, swallowing, and even autonomy in daily living activities.
When rehabilitation takes place remotely through digital tools and telecommunications, it is referred to as telerehabilitation.
What technologies are used in telerehabilitation?
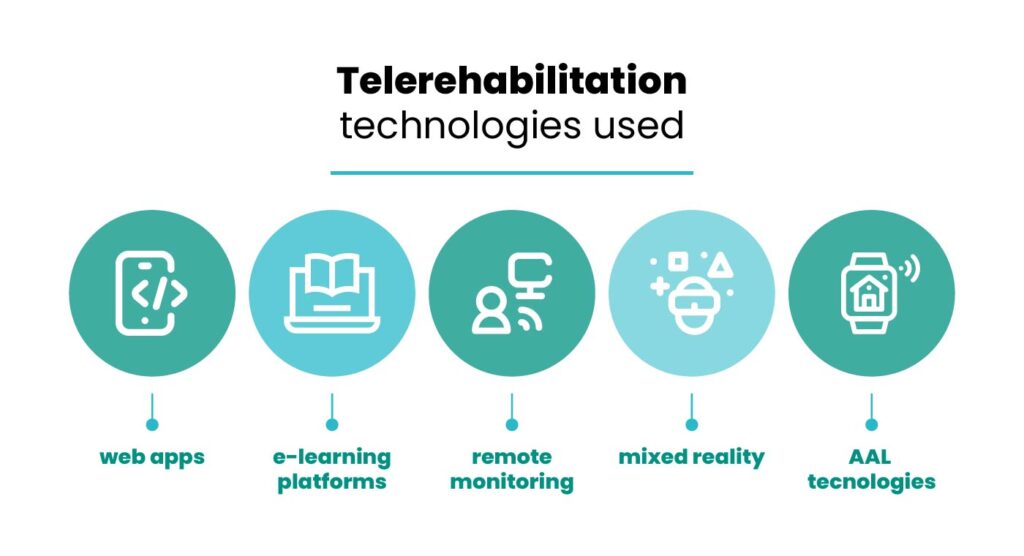
Here are some examples of technologies used in telerehabilitation:
- video call platforms for live sessions between therapist and patient;
- web apps for motor or cognitive exercises to be performed at home:
- e-learning platforms for cognitive rehabilitation;
- virtual reality (VR) and augmented reality (AR) to create immersive environments where motor activities can be simulated;
- remote monitoring to assess parameters such as movement, posture, and balance;
- AAL technologies, such as interfaces for patients with motor and cognitive disabilities.
Cognitive telerehabilitation
Cognitive telerehabilitation is aimed at patients with neurological disorders, post-stroke conditions, traumatic brain injuries, mild cognitive impairment (MCI), and dementia. The goal is to restore or maintain functions such as memory, attention, and language, while strengthening residual abilities.
It is often delivered through:
- online courses with personalized cognitive exercises;
- VR simulations;
- continuous remote monitoring with regular specialist feedback.
How long does a rehabilitation program last?
The duration of a rehabilitation program depends on several factors:
- type of condition: whether it is acute, chronic, progressive, or stable;
- therapeutic goal: complete recovery, functional improvement, maintenance, or compensation;
- severity and stage of the condition: for example, recovery may be much faster in the early stages after a stroke;
- frequency of sessions, method (in-person/remote), and the patient’s commitment outside guided sessions.
There is no fixed number of weeks or months that can be applied universally. In Italy, experimental projects in cognitive telerehabilitation often include cycles of several weeks (for example, 6–12 weeks) with sessions 2 to 3 times per week, but they may extend much longer, especially in the case of chronic conditions.
Benefits, challenges, and future outlook
Telerehabilitation helps overcome geographical barriers, improves access to care, and ensures greater continuity of treatment even when patients cannot attend clinics in person. For people living in remote areas or with reduced mobility, it represents added value that can translate into time and cost savings.
However, there are still challenges: inadequate internet access, the need for suitable technological devices, ongoing training for healthcare professionals, data protection and privacy issues, and the requirement for healthcare facilities to adopt clear protocols and updated guidelines are urgent matters that must be addressed.
Looking ahead, greater integration of telerehabilitation into local healthcare systems is expected, supported by public policies and funding aimed at promoting a balanced spread of these care models.
Contact us to develop your project
Telerehabilitation today represents an effective and innovative solution to ensure equity, continuity, and quality of care.
If you represent an organization, institution, research center, or company interested in developing European projects focused on telerehabilitation — from needs analysis to design, implementation, and validation — get in touch with us. We can support you.
Reach out today or send us an email to explore funding opportunities, partnerships, and tailored solutions: take the next step toward the future of rehabilitation with IPPOCRATE AS.

